This blog is the first in a series of three instalments, followed by Part 2 (Clinical Overview & Diagnosis) and Part 3 (Therapy & Treatment).
Pyoderma is a skin infection caused by pyogenic bacteria, usually Staphylococci, and is one of the most frequent diseases in veterinary dermatology. It is characterised by a pleomorphic clinical presentation, which can often mimic many other skin diseases such as demodicosis, dermatophytosis or pemphigus foliaceus. Rarely occurring as a primary form, in most cases it
represents a complication of a pre-existing disease, such as atopy, food allergy, horny disorders, parasitic diseases, endocrinopathies and immunodeficiency states.
Ethyology
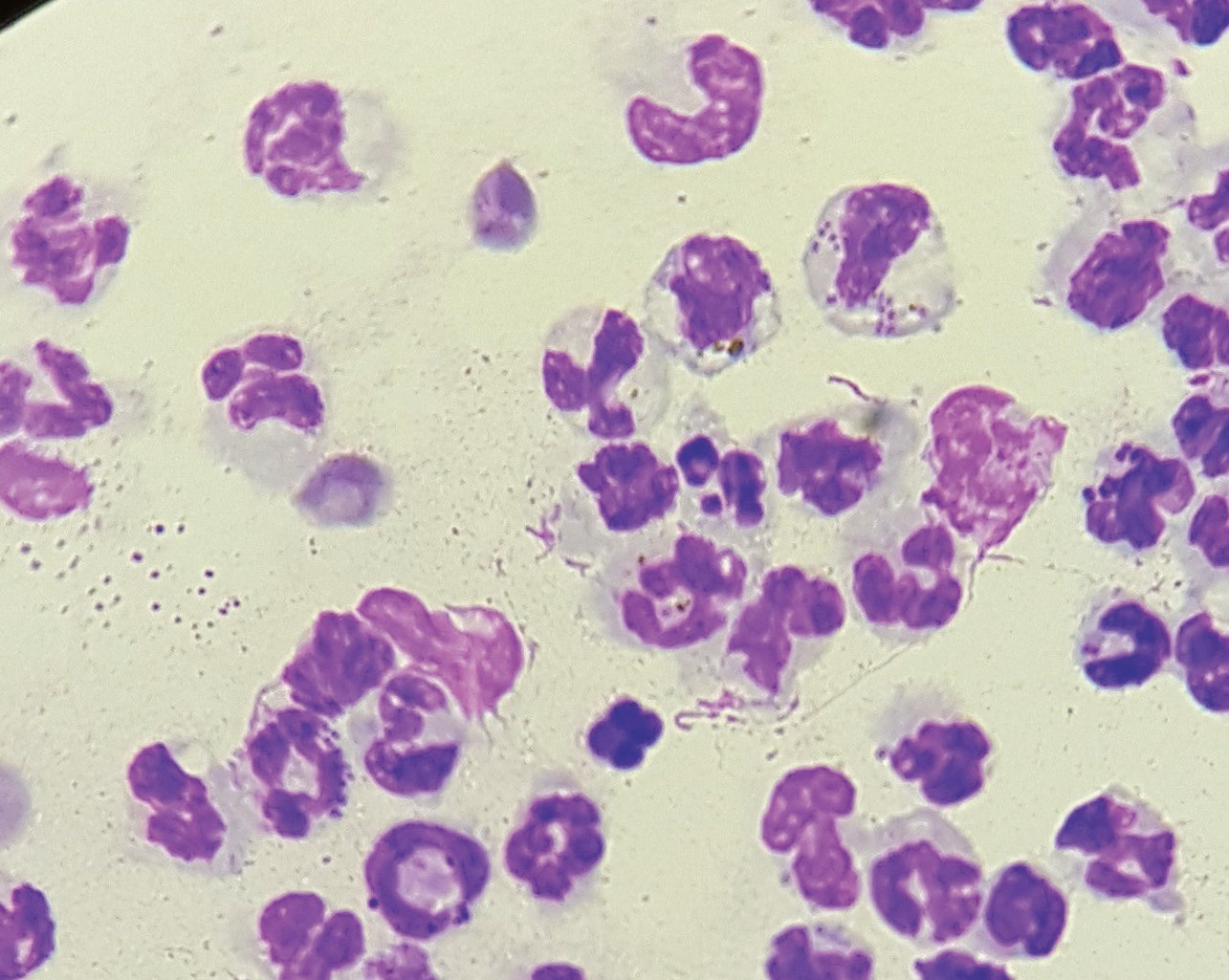
Ninety per cent of pyoderma in dogs is caused by Staphylococcus pseudointermedius, a Gram positive bacterium, coagulase-positive and beta-haemolytic.
However, other coagulase-positive and -negative staphylococci species, and other Gram-positive and -negative bacteria such as Pseudomonas aeruginosa or Enterobacteriaceae such as Proteus and Escherichia coli are occasionally isolated.
Staphylococcus pseudointermedius and other bacteria are usual residents of the skin and/or mucosae and can colonise them without causing disease. In some circumstances, these bacteria are able to multiply excessively and become pathogenic thanks to a variety of enzymes and toxins (virulence factors) that encourage colonisation and infection.
Among the best known are the toxin TSS-1 (Toxic Shock Syndrome-1 produced by S. aureus), responsible for toxic shock syndrome in human; protein A (produced by S. aureus and S. intermedius), which binds to the Fc fraction of immunoglobulins and has a potent pro-inflammatory action; coagulase (produced by S. aureus, S. intermedius, S. hycus), which by encouraging deposition of fibrin on bacterial cells makes their identification by phagocytes more difficult; and β-lactamase, enzyme responsible for the resistance to non-protected penicillins.
Pathogenesis of the infection
Healthy skin has many protective mechanisms that prevent the penetration of pathogens. The stratum corneum, with its continuous desquamation and consequent elimination of microorganisms adhered to the surface, represents the first effective barrier. The hydrolipidic film, produced by sebaceous glands, keratinocytes and apocrine glands, permeates the intercellular spaces and follicular ostia, and contains nutrients for some resident microorganisms and inhibiting substances for other pathogens, as well as cytokines, complement and immunoglobulins that are able to inhibit bacterial enzymes and toxins.
The skin microflora is a mixture of resident bacteria and yeasts, which constitute the microbiota. Under normal conditions, these non-pathogenic microorganisms compete with pathogenic ones for nutrients and developmental niches and, together with the host's defence systems, prevent their proliferation.
However, in dog there are anatomical features that make it more prone to skin infections than other species. The stratum corneum is thinner and more compact, and intercellular spaces are permeated by a lesser amount of hydro-lipid film, and the follicular osti are devoid of this protective emulsion and are beants.
Pyoderma develops whenever the skin balance is perturbed. It is in fact rarely a primary disease; it occurs more frequently as a secondary infection in case of skin, metabolic and immunological anomalies. Allergic diseases, keratinisation disorders, ectoparasite infestations and metabolic and endocrine disorders are the most frequent predisposing causes. Allergy patients in particular are predisposed to secondary pyoderma due to the intrinsic deficiency of long-chain ceramides in the intercellular lipids of the stratum corneum, resulting in a defect of the protective surface barrier.
In addition, itching causes continuous self-induced skin excoriations that worsen the protective barrier defect. Inflammation due to allergy or self-induced lesions can further disrupt the skin barrier due to the passage of exudate via the transepidermal route. This increase in permeability allows the passage of seric components from the blood vessels to the skin surface, which is then enriched with nutrients for bacteria.
The bacterial population on the skin surface of atopic subjects appears to be more numerous than that of normal subjects, and mainly consisting of staphylococci, as the corneocytes of allergic dogs allow better adhesion to the bacteria. Finally, the anti-itch therapy to which allergic
animals are often submitted may cause a decrease in the efficiency of the host's immune system and encourage infection.
High humidity and temperature favour an increase in the bacterial load in the skin. Poorly aerated skin areas, such as the axillary and interdigital region or skin folds of the face and vulva,
retain humidity and have higher temperatures. This explains why superficial pyoderma is mainly
localised in these sites and why in humid climates and during summer there is a higher incidence of skin infections, especially in dogs with long, thick hair (Chow Chow, German Shepherds, Bobtails, etc.).
On the other hand, excessive dryness of the skin can also lead to an imbalance in the surface ecosystem and encourage infections. The presence of seborrhoea and hornification disorders in
general, due to abnormalities in the production of the corneal barrier and protective lipid film, make it easier to set up an infection.
In some hornification defects, such as primary seborrhea, the comedonic syndrome of the Schnauzer and sebaceous adenitis, follicular obstructions (comedones, follicular moulds) occur that promote the development of bacterial folliculitis. Other causes of inflammation and follicular obstruction predispose to bacterial follicle infections. Among these the most frequent are demodicosis and dermatophytosis.
Follicular obstruction and bacterial folliculitis are also observed during hormonal diseases, such as hypothyroidism or hyperadrenocorticism. Furthermore, hormonal imbalances are often linked to states of secondary immunodepression and can therefore predispose to recurrent pyoderma, particularly in elderly subjects. In general, all states of immunodepression, whether congenital, acquired or iatrogenic, favour skin infections.
 UK
UK

 Global English
Global English