When is the best time to do allergen-specific IgE serological testing?
This question is commonly asked by veterinarians to Nextmune colleagues, and I could simply reply that there are no studies in the literature that unequivocally address this question.
Nevertheless, I can foresee at least three factors, two of them overlapping, that could influence when to run the test for the best chance to obtain optimal results. These factors are: 1) the stage of atopic disease activity, 2) the pollination season and, 3) vaccination boosters.
Let’s explore the rationale of how each of these factors could affect the results of IgE serology.
1. the stage of atopic disease activity
The critical point here is to test shortly (1-4 weeks) after an acute flare of the disease, which indicates that there has been recent contact with the offending allergen(s); this should lead to an elevation in the offending allergen-specific IgE.
It is self-evident that testing a dog with a summer-worsening atopic dermatitis in the middle of winter makes little sense, as the disease flares are likely pollen-triggered, and this dog would have had no contact with pollens for months. Remember that, in humans and likely in other mammals, the serum half-life of IgE is only 2 days, meaning that, without any stimulation of their production after an allergen contact, levels of allergen-specific IgE will rapidly disappear from the circulation.
We have verified in our allergic dog model that, without allergen challenges, serum allergen-specific IgE rapidly decreases—sometimes to negative levels—while the topical allergen provocation (or even a simple intradermal test) will rapidly increase the secretion of the corresponding allergen-specific IgE!
Beware of chronic atopic dermatitis! There is a vicious circle of inflammation in such a disease stage in which cells keep activating each other, eventually without needing any IgE or allergen contact. You might have a negative IgE serology in such a situation due to a lack of recent allergen contact.
Remember: an acute flare would be needed to have the highest chance of detecting serum allergen-specific IgE!
2. the pollination season
Years ago, I had the opportunity to look at the average levels of allergen-specific IgE, month per month, in thousands of dogs whose sera had been submitted to an allergy diagnostic laboratory in Japan (Animal Allergy Clinical Laboratory, courtesy of Dr. Ken Masuda). The data clearly showed that the average levels of a pollen-specific IgE begin increasing shortly after its pollination season, and pollen IgE levels are lowest in the winter. Interestingly, the same summer rise phenomenon was observed for house dust mite-specific IgE, which is also to be expected as mites proliferate more in seasons of higher temperatures and humidity.
As a result, it seems logical to perform IgE serological testing during the seasons in which patients’ signs flare – this recommendation thus coincides with that made above.
3. vaccinations
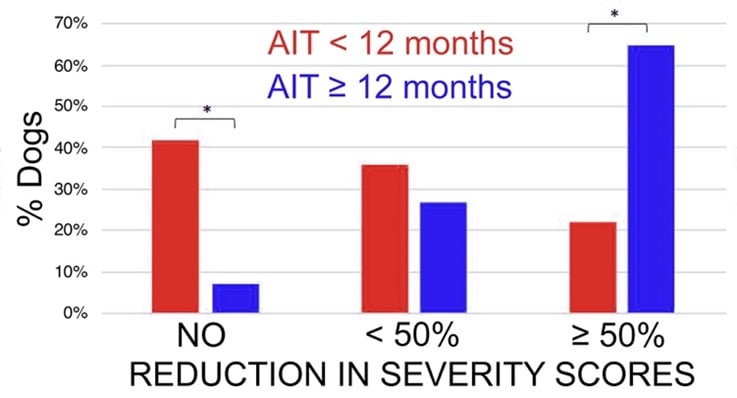
A decade ago, previous colleagues at NC State University showed, using our allergic dog model, that a typical routine vaccination led to an increase in IgE and IgG specific for corn, the allergen to which the dogs were sensitized, between 1 and 3 weeks after vaccination. IgE levels returned to normal by 8 weeks after injection (Tater, Amer J Vet Research 2005).
A few years later, I confirmed that a routine vaccination, in other dogs from the same colony, induced a rise in beef-, lamb- and milk-specific IgE. This was not surprising as bovine serum albumin has been shown previously to be present in vaccines and triggers specific IgE production (Ohmori, Vet Immunol 2007). Importantly, we also showed a rise in serum IgE directed against an allergen to which the dogs were sensitized at that time (e.g., Japanese cedar pollens). Finally, we also detected, post-vaccination, specific IgE directed against allergens to which the dog had not been sensitized experimentally (e.g., Alternaria molds and others)! Thus, it is clear that a routine vaccination rapidly induces the production of multiple allergen-specific IgE!
Unfortunately, I remain perplexed about what to do with these results. On the one hand, one might want to avoid testing rapidly after vaccination to decrease non-specific IgE detection probability. On the other hand, one could wish to test soon after vaccination to pick up antibodies released from vaccine-activated clones of B and plasma cells previously committed to allergen-specific IgE production. Clearly, this is an area deserving of further study.
So, to answer the question raised by our colleagues about when to submit blood for allergen-specific IgE, I would reply the following:
- Test during the season(s) known to trigger the flares, and/or
- Test within a month after an acute flare of the disease, and
- Beware of the effect of vaccination on your serological test results. If you document a rise in allergen-specific IgE that does not correspond to the pattern of clinical reactivity of your patient, you might want to not give them much importance.
 UK
UK

 Global English
Global English
-Dec-21-2023-09-46-12-9148-AM.jpeg)