What should I choose: intradermal testing or IgE serology?
Dear Colleagues,
At the beginning of 2021, I would like to begin by wishing you a Happy New Year! May this new year be better than the last one, and may the SARS-CoV-2 vaccines that are starting to be distributed in our countries bring a sense of normalcy as soon as it is immunologically feasible!
Now, back to allergy and dermatology! In this newsletter, I would like to continue answering a question from the list of those commonly asked by veterinarians to Nextmune colleagues.
When I want to start allergen immunotherapy in a dog, should I do—or refer to a specialist for—an intradermal test (IDT), or should I submit blood for IgE serology?
Let me start by providing some background on these two tests.
At this time, in animals, skin testing is done either by intradermal injections (most commonly) or prick testing (more rarely). Both methods result in the iatrogenic introduction of a small amount of a protein mixture from an allergen source into the superficial dermis. There, culprit allergens cross-link two allergen-specific IgE lying on their high-affinity receptor on the surface of mast cells. Such a cross-linking induces receptor activation and cellular degranulation to release numerous mediators, including histamine, among others. The histamine then activates the H1R receptors on endothelial cells, which results in their contraction and the ultimate extravasation of plasma into the dermis. Clinically, a positive reaction is seen as an erythematous wheal that rapidly occurs after allergen challenge.
The IgE serology generally consists of an ELISA for multiple allergens that are coated onto a plate. After a blocking step, the serum of allergic patients is diluted and incubated onto the coated allergens. Subsequently, an enzyme-coupled IgE-specific reagent, be it a recombinant high-affinity IgE receptor chain, a single or several monoclonal antibodies, or a polyclonal antiserum, is added. Finally, an enzyme substrate allows a colorimetric reaction to occur to permit the measurement of allergen-specific IgE.
Intradermal and serological tests are not tests to diagnose a clinical allergy. Instead, both evaluate the status of a patient's IgE sensitization in two different tissues: the skin (for the intradermal test) and the peripheral blood (for the serological test). Furthermore, both tests evaluate the IgE sensitization within two different time frames. Indeed, it is essential to know that the half-life of IgE in the blood is 2-to-3 days, while that on skin mast cells is between 16 and 20 days (both are values in humans). As a result, one needs to look at the IgE serum levels as a biomarker for a recent (i.e., days) IgE secretion by plasma cells. In contrast, the IDT represents a biomarker of an earlier (i.e., weeks) and sustained IgE production.
This dual time frame is similar, in concept, to the evaluation of glucose metabolism using blood levels of either glucose (as a biomarker for recent glucose metabolism) or fructosamine (for a biomarker of the glycemia in the preceding month). In this comparison, the IgE serology would correspond to the blood glucose measurement, while the IDT would be the fructosamine level. When there is a sustained and persistent allergen contact, the IgE serology and IDT results will often correlate; they might not if such contact were episodic, however.
I had a first-hand experience of this phenomenon when experimentally-sensitizing atopic dogs to pollen and house dust mite allergens.
In the figure below, I represented a typical situation that occurred when we sensitized our dogs to, let's say, Dermatophagoides farinae house dust mites. We usually started with weekly topical applications of a mite powder in mineral oil (red arrows). After skin reactions became visible after an allergen challenge, we then spaced the "booster" applications. In one experiment, we measured three immunological parameters during sensitization. The first biomarker of a successful sensitization was the proliferation of blood T cells when cultured with mite allergens. This lymphocyte activation occurred rapidly (blue line) and then faded before plateauing. Serum mite allergen-specific IgE (red line) were detectable within a few weeks of sensitization, but, interestingly, levels often decreased in the absence of an allergen contact. However, after a further allergen challenge, serum mite-specific IgE titers increased rapidly, likely reflecting the presence of allergen-specific IgE-committed memory B cells in the blood. Finally, it generally took weeks of sustained serum IgE elevation for the IDT (green) to become positive. At first, this test was only positive to high concentrations of allergens, and then, later, to ten-fold lower amounts of allergens, likely reflecting the presence of increasing levels of specific IgE on the skin mast cell membranes.
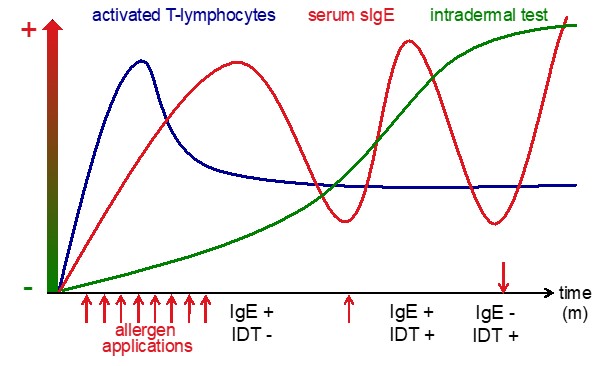
Now here is where IDT and specific-IgE come together! If we were to perform both tests at different periods, one would have variable test results! During the first period (leftmost pink box), the IgE serology would be the only positive. In the middle period (box), both tests would be so. Weeks after an allergen contact (rightmost box), the IDT might be the only yielding positive results!
This was an example of a controlled situation with a single allergen sensitization. Now, think of one of your pet patients that had on-and-off contacts with environmental allergens. When you decide to perform an IDT or IgE serology, most of the time you will not know when were its latest contacts with offending allergens! As a result, you could be in any of the three situations above for each of the allergens tested!
I know this was a lengthy diatribe before answering the original question… So, which test should you choose? The answer is self-evident: “If you can, and the owner can afford it, do both tests!” Having both results would allow for a clearer picture of your patient's sensitization status. If you can only do one test, choose either, knowing that the results will represent only one phase of the patient's sensitization status.
I hope that my lengthy explanation will also help understand why comparing IDT and serology results in a patient at a single time would be like comparing apples and oranges. Finally, I wish I illustrated the concept that the IDT is no more a gold standard than the IgE serology is - they both are sensitization standards, just different ones!
Again, best wishes for 2021 to all of you!
Till next month!
Respectfully submitted,
Thierry Olivry, DrVet, PhD, DipECVD, DipACVD
Research Professor of Immunodermatology
NC State University College of Veterinary Medicine, Raleigh, North Carolina, USA
Scientific Advisor and Dermatology & Allergy Consultant
Nextmune, Stockholm, Sweden
 UK
UK

 Global English
Global English
-Dec-21-2023-09-46-12-9148-AM.jpeg)